Relationship Between Heart Rate Variability Parameters and Short-Term Prognosis of Patients with Acute Myocardial Infarction
By Chun-Mei Wang1, Tao-Tao Su2, Yang Yue2, Wei-Xing Han1Affiliations
doi: 10.29271/jcpsp.2024.04.468ABSTRACT
Objective: To determine the link between heart rate variability (HRV) and short-term adverse outcomes (re-hospitalisation or death due to cardiac arrhythmia, recurrent myocardial infarction, heart failure, all-cause death) in acute myocardial infarction (AMI).
Study Design: A descriptive study.
Place and Duration of the Study: Department of Cardiovascular Medicine, The First Affiliated Hospital of Anhui Medical University, China, from January 2018 to December 2021.
Methodology: Clinical data of 245 patients diagnosed with AMI were retrospectively analysed. After discharge from the hospital, patients were followed for a year and categorised into two groups based on the occurrence of adverse events: the adverse event group (n=82) and the no adverse event group (n=163). Differences in clinical characteristics were compared, independent factors influencing adverse events were analysed, and diagnostic efficacy was assessed.
Results: Univariate analysis showed age, hyperlipidaemia, specific HRV parameters (SDNN, SDANN, RMSSD, PNN50, LF/HF), and myocardial injury markers (CK-MB, cTnI, NT-proBNP) as associated with these events (all p < 0.05). Multivariable analysis revealed decreased SDNN, decreased SDANN, increased LF/HF, and elevated levels of CK-MB, cTnI, and NT-proBNP as independent influences. Both HRV parameters and myocardial injury markers were reliable predictors on ROC curve analysis. The highest diagnostic efficacy was achieved by combining these predictors.
Conclusion: AMI patients frequently experience short-term adverse events. Both HRV parameters and myocardial injury markers, which demonstrate significant predictive efficacy, independently influence these outcomes.
Key Words: Acute myocardial infarction, Coronary angiography, Heart rate variability, Myocardial injury, Risk factors.
INTRODUCTION
Acute coronary syndrome (ACS) is one of the major causes of death worldwide, with a mortality rate of 7.1%. Among these cases, acute myocardial infarction (AMI) is the most common diagnosis.1 Previous theoretical studies and clinical practice have demonstrated that the prognosis of AMI and myocardial injury markers (CK-MB, cTnI, NT-proBNP) are significantly correlated.2-4 Patients have a poor long-term prognosis and a significantly increased risk of adverse endpoint events in the short term. Dynamic electrocardiograms might be another option for assessing the prognosis of AMI.
HRV refers to the variability between each cardiac cycle, which primarily reflects the dynamic balance of cardiac autonomic regulation, serving as a complex and sensitive indicator of the cardiac autonomic system. HRV can be clearly recorded by an ECG. Available literature reports that HRV may play an important role in assessing the correlation between coronary artery injury and autonomic nervous system dysfunction.5 Since markers of myocardial injury also offer the advantages of being easy to obtain with rapid and reliable results, both HRV parameters and myocardial injury markers are vital for the prognostic assessment of coronary artery disease, particularly in AMI patients, and for early and active intervention.
This study retrospectively analysed the expression of HRV parameters and markers of myocardial injury in AMI patients with different prognoses. The aim of the study was to analyse the relationship between HRV parameters and markers of myocardial injury and adverse endpoint events and the predictive efficacy of both for adverse endpoint events.
METHODOLOGY
The clinical data of 245 patients who were admitted to the Department of Cardiovascular Medicine at the First Affiliated Hospital of Anhui Medical University with heart pain and chest tightness, and were diagnosed with AMI through coronary angiography, were analysed. The data was retrieved from the hospital’s electronic medical records system from January 2018 to December 2021. Eligible participants for this study were individuals aged 18 years and above, with no prior history of cardiac stent placement. All participants had to be diagnosed with AMI through a combination of clinical presentation, alterations in myocardial enzymes, and findings from electrocardiographic and imaging studies. The study, however, excluded individuals with hypertrophic cardio-myopathy and those who had concurrent malignancy, haematological disorders, or severe infectious diseases. Also, patients with a recent history of significant surgery, or those who had been subjected to hormone or immunosuppressive shock therapy were excluded. The study additionally required that all participant data be complete. Uncooperative individuals or those who declined participation were also exempted from the study.
All patients were admitted to the hospital and underwent relevant examinations, including Holter-ECG, 24-h ambulatory blood pressure test, blood biochemistry and cardiac ultrasound, and then coronary angiography after completing the relevant examinations. The HRV parameters included the overall standard deviation of all normal RR intervals (SDNN), the standard deviation of the mean RR intervals (SDANN), the standard deviation of all NN intervals for all 5-minute segments (288) of 24 hours (SDANN Index), and the number of adjacent RR intervals with a difference of more than 50 ms. (PNN50), the root mean squared (RMSSD) triangular index (TRIIDX) of the difference between adjacent RR intervals over the whole time, and the frequency domain indices: low frequency (LF), high-frequency (HF), and low frequency/high frequency ratio (LF/HF).
AMI was diagnosed accordingly with reference to the relevant clinical nomenclature and diagnostic criteria of the American Heart Association (AHA) and the American College of Cardiology (ACC).6 Based on the 12-month follow-up, patients in the AMI group were divided into an adverse event group (n=82) and a no adverse event group (n=163).
All AMI patients were given standardised treatment and prophylaxis, including thrombolysis and reperfusion therapy according to time of onset, antiplatelet therapy, anticoagulation, aspirin, beta antagonists, ACEI (ARBs for those who cannot tolerate ACEI), statins (depending on the patient’s lipid level), and secondary prophylaxis.
Data were analysed using the IBM-SPSS 26.0 software package, and normality tests were performed using the Kolmogorov-Smirnov method. Econometric data were expressed in (x±s) and statistically analysed using Student’s t-test for two independent samples; count data were statistically described using composition ratio or rate and statistically analysed using χ2 test. Multifactorial analysis was processed using unconditional dichotomous logistic regression analysis. ROC curves were analysed for the diagnostic value of HRV parameters, markers of myocardial injury, and HRV parameters combined with markers of myocardial injury. A p <0.05 was the test level.
RESULTS
The age of all the patients ranged from 35 to 86 years, with an average of 56.85±8.75 years. The group included 120 males and 125 females. Differences between general clinical information, HRV parameters, and markers of myocardial injury were compared between the adverse event and no-adverse-event groups, respectively. The results demonstrated that age, LVEF, hyperlipidaemia [total plasma cholesterol ≥5.17 mmol/L (200 mg/dL), triglycerides 1.7 mmol/L (150 mg/dL), HDL cholesterol <1.04 mmol/L (40 mg/dL) or LDL cholesterol >3.37 mmol/L (130 mg/dL)], HRV parameters (SDNN, SDANN, PNN50, RMSSD, LF/HF), and markers of myocardial injury (CK-MB, cTnI, NT-proBNP), and adverse endpoint events were statistically significant (all p <0.05, Table I).
Table I: Univariate analysis affecting the occurrence of adverse events [(x̄±s), cases (%)].|
Parameter |
Adverse events group (n=82) |
No adverse event group (n=163) |
t/χ2 |
p |
|
Gender (male / female) n (%) |
40 (48.8) / 42 (51.2) |
80 (49.1) / 83 (80.9) |
0.002 |
0.965 |
|
Age ≥60 years (Yes/No) n (%) |
61 (74.4) / 21(25.6) |
43 (26.4) / 120 (73.6) |
51.473 |
<0.001 |
|
Hyperlipidaemia (Yes/No) n (%) |
45 (54.9) / 37 (45.1) |
22 (13.5) / 141 (86.5) |
47.019 |
<0.001 |
|
Diabetes (Yes/No) n (%) |
30 (36.6) / 52 (63.4) |
60 (36.8) / 103 (63.2) |
0.001 |
0.973 |
|
LVEF (%) |
69.80±5.55 |
71.85±6.15 |
2.542 |
0.012 |
|
HRV parameters |
|
|
|
|
|
SDNN (ms) |
(77.85±7.21) |
(81.09±5.95) |
3.732 |
<0.001 |
|
SDANN (ms) |
(69.01±6.01) |
(71.69±7.18) |
2.910 |
0.004 |
|
SDANN Index |
(42.82±2.01) |
(43.37±3.85) |
1.199 |
0.232 |
|
TRIIDX |
(30.82±3.33) |
(31.14±3.28) |
0.695 |
0.488 |
|
RMSSD (ms) |
(20.37±4.08) |
(22.31±7.30) |
2.241 |
0.026 |
|
PNN50 (%) |
(9.53±1.40) |
(10.41±3.05) |
2.494 |
0.013 |
|
LF/HF |
(1.15±0.06) |
(1.04±0.29) |
3.257 |
0.001 |
|
Markers of myocardial injury |
|
|
|
|
|
CK-MB (ng/mL) |
(29.39±6.33) |
(26.82±4.07) |
3.850 |
<0.001 |
|
cTnI (μg/L) |
(1.45±0.78) |
(1.23±0.26) |
3.303 |
0.001 |
|
NT-proBNP (ng/mL) |
(3374.76±581.91) |
(3026.99±404.58) |
5.452 |
<0.001 |
|
P:χ2 test was used for gender, age, hyperlipidaemia, diabetes, and Student’s-t test was used for other parameters. |
||||
Table II: Multifactorial logistic regression analysis affecting the occurrence of adverse events in patients with AMI.
|
Parameter |
β |
SE |
Wald |
p |
OR |
95%CI |
|
Age ≥60 years old |
1.782 |
0.392 |
20.640 |
<0.001 |
5.944 |
2.755~12.825 |
|
Hyperlipidaemia |
2.017 |
1.314 |
2.356 |
0.125 |
7.513 |
0.572~98.688 |
|
SDNN (ms) |
-0.062 |
0.030 |
4.328 |
0.038 |
0.940 |
0.887~0.996 |
|
SDANN (ms) |
-0.064 |
0.030 |
4.645 |
0.031 |
0.938 |
0.885~0.994 |
|
LF/HF |
2.234 |
0.978 |
5.214 |
0.022 |
9.334 |
1.372~63.488 |
|
CK-MB (ng/mL) |
0.146 |
0.040 |
13.316 |
<0.001 |
1.157 |
1.070~1.252 |
|
cTnI (μg/L) |
0.635 |
0.305 |
4.335 |
0.037 |
1.887 |
1.038~3.430 |
|
NT-proBNP (ng/mL) |
0.001 |
0.000 |
7.520 |
0.006 |
1.001 |
1.000~1.002 |
|
Constant |
-7.583 |
3.791 |
4.001 |
0.045 |
0.001 |
— |
The variables deemed significant for the univariate analysis (including age, hyperlipidemia, LVEF, SDNN, SDANN, RMSSD, PNN50, LF/HF, CK-MB, cTnI, and NT-proBNP) were used as independent variables. The presence or absence of adverse endpoint events (1 for presence and 0 for absence) were used as the dependent variables for unconditional dichotomous logistic regression analysis.
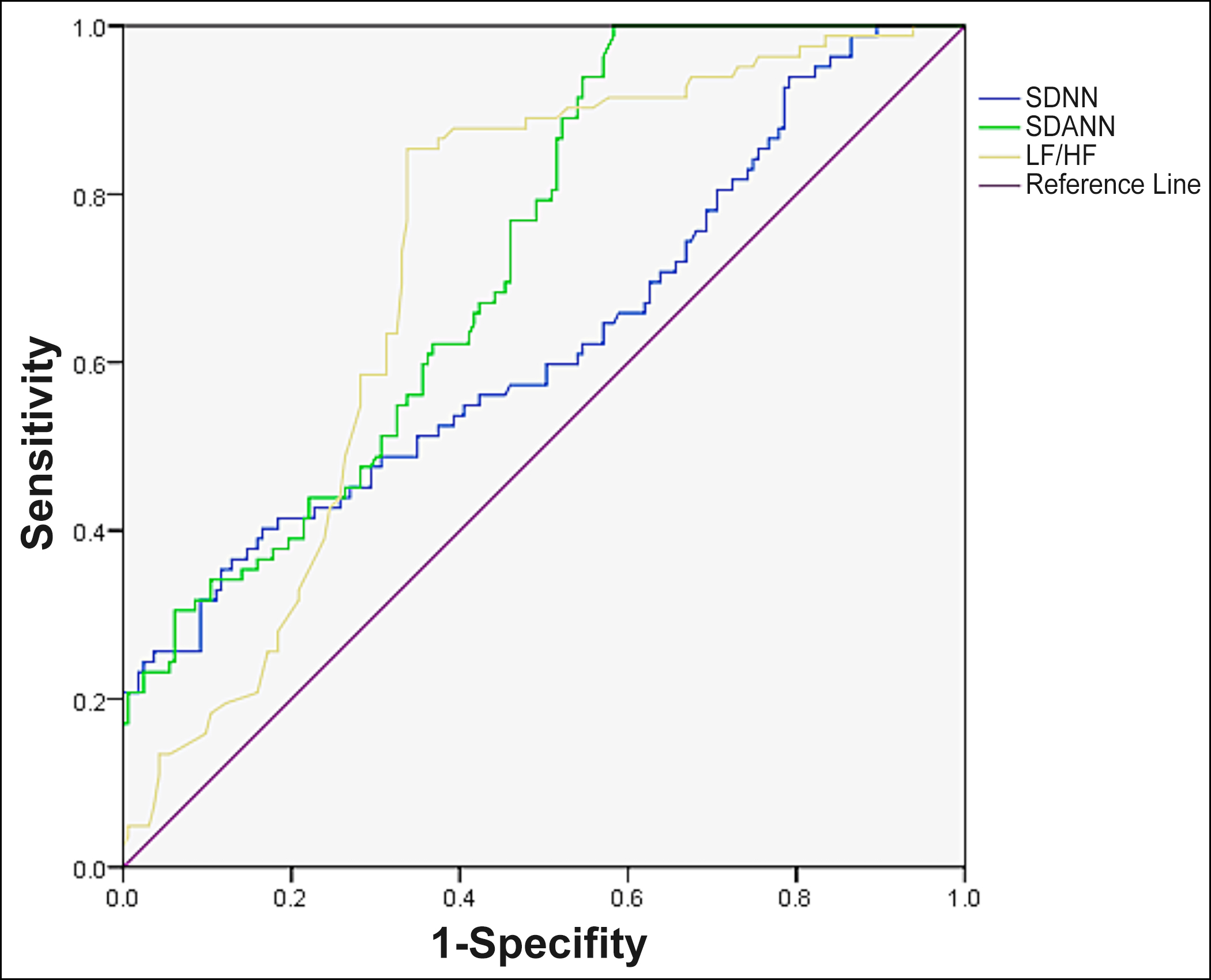 Figure 1: Predictive value of HRV parameters for the occurrence of short-term adverse endpoint events in patients with AMI.
Figure 1: Predictive value of HRV parameters for the occurrence of short-term adverse endpoint events in patients with AMI.
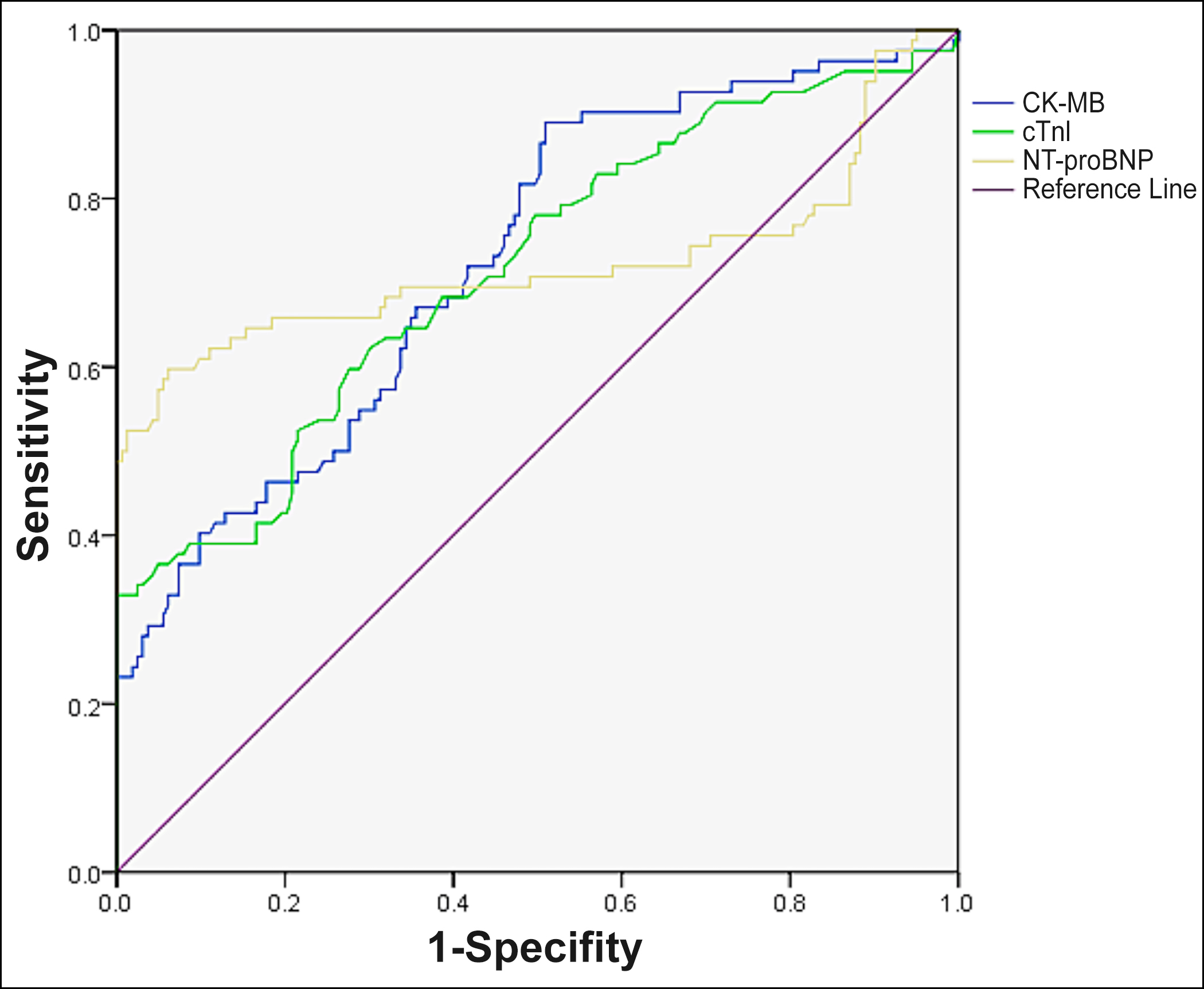 Figure 2: Predictive value of myocardial injury markers for the occurrence of short-term adverse endpoint events in patients with AMI.
Figure 2: Predictive value of myocardial injury markers for the occurrence of short-term adverse endpoint events in patients with AMI.
The optimisation model was fitted using the stepwise backward method for analysis. The results showed that age ≥60 years, hyperlipidaemia, decreased SDNN, decreased SDANN, elevated LF/HF, elevated CK-MB, elevated cTnI, and elevated NT-proBNP were independent risk factors for the occurrence of adverse endpoint events in patients with AMI (all p <0.05). The results are shown in Table II.
The ROC curves of HRV parameters (SDNN, SDANN, LF/HF), myocardial injury markers (CK-MB, cTnI, NT-proBNP), and HRV parameters combined with myocardial injury markers to predict the occurrence of adverse endpoint events were plotted separately (Figures 1-3). The results showed that HRV parameters, myocardial injury markers, and the combined test had some predictive value for the occurrence of adverse events in AMI patients, however, the highest diagnostic efficacy was found by using the combined test (AUC = 0.868, 95% CI:0.821~0.915, p <0.001). The sensitivity and specificity of the combined diagnosis were 0.732 and 0.859, respectively.
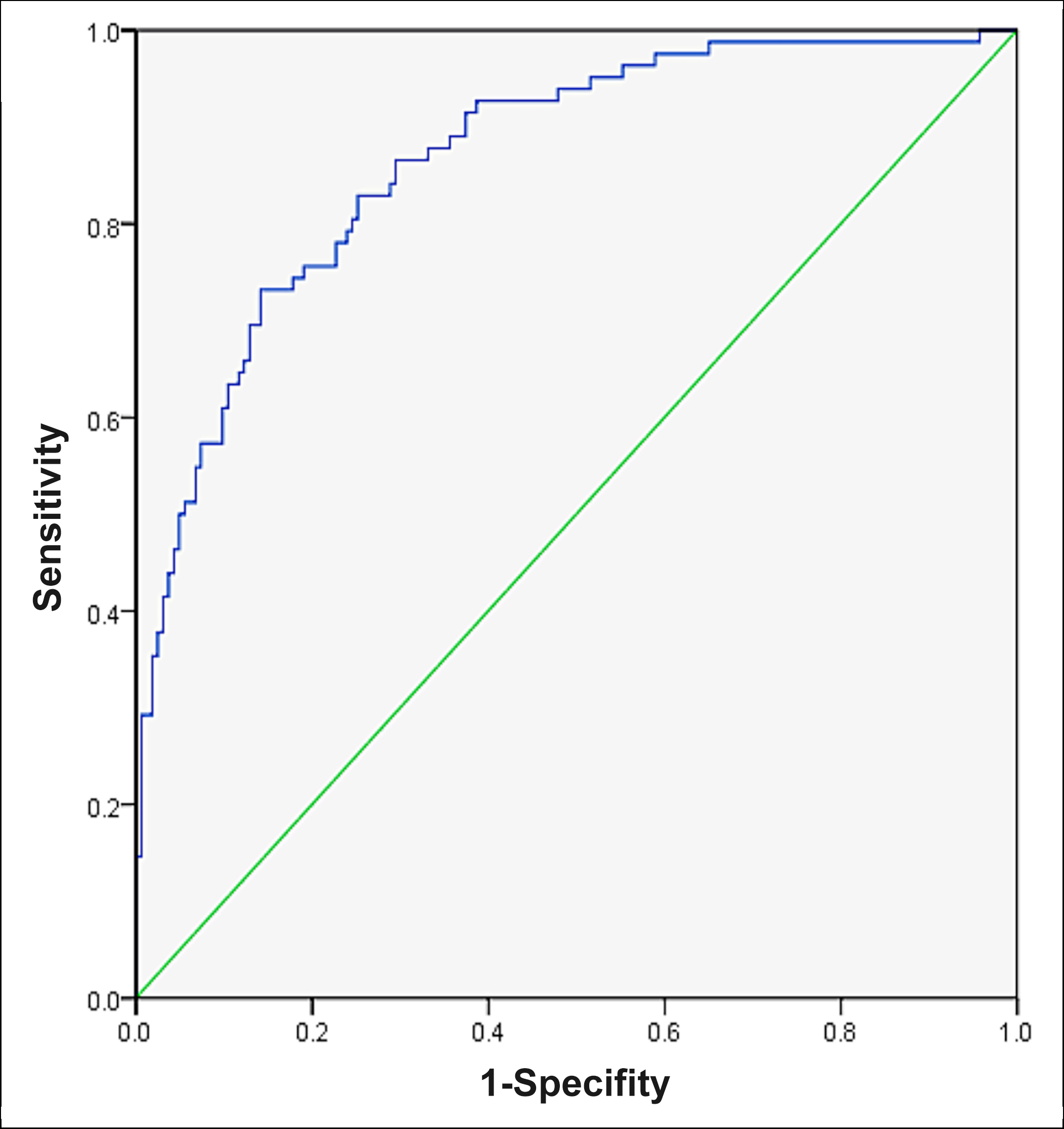 Figure 3: Predictive value of the combined diagnosis for the occurrence of short-term adverse endpoint events in patients with AMI.
Figure 3: Predictive value of the combined diagnosis for the occurrence of short-term adverse endpoint events in patients with AMI.
DISCUSSION
Coronary heart disease (CHD) stands as a leading cause of death worldwide, accounting for approximately 7.4 million deaths annually.7 Particularly, patients with CHD, especially those with AMI, are at high risk for short-term adverse events. These adverse events predominantly include non-fatal myocardial infarction, heart failure (HF), non-fatal stroke, all-cause mortality, and emergency coronary artery revascularis ation.8,9 Despite the tremendous advances in the treatment of AMI in modern medicine, represented by emergency PCI, the prognosis of AMI has not gained significant changes in the past decades.10 Many AMI patients present with adverse events, such as recurrent myocardial infarction, death from heart failure, or all-cause mortality soon after hospital discharge. Previous studies on risk factors for adverse events in AMI patients have mostly focused on patients' general clinical symptoms, laboratory tests, past medical history, and surgical conditions, and there is a lack of multicentre, large-sample studies on the correlation between HRV parameters obtained by ambulatory electrocardiography and adverse endpoint events. Therefore, this study has good clinical significance in selecting HRV parameters for predicting the incidence of short-term adverse events in patients with AMI.
Patients with AMI present with acute ischemic injury to cardiac myocytes, altered overall synergy of cardiac contraction and cardiac myocyte conduction, and impaired cardiac autonomic regulation. HRV is the only noninvasive quantitative response to cardiac autonomic nervous system function, and it reflects a balanced relationship between sinus node regulation and the interaction of neurohumoral factors. Previous studies have confirmed that HRV can predict the risk of cardiac events.11 The present study shows that the HRV parameters SDNN, SDANN, and LF/HF are independent influences on the occurrence of adverse endpoint events in AMI patients in the short term SDNN reflects the total activity of vagus and sympathetic nerves, and a decrease in the SDNN test indicates a decrease in the overall autonomic tone. SDANN is mainly used to assess sympathetic activity, and a decrease in its test value indicates an increase in sympathetic tone. LF/HF, on the other hand, reflects the state of sympathetic and vagal nerve dynamic balance. In this study, the SDNN and SDANN values of patients in the adverse event group were significantly lower than those of patients in the non-adverse event group, while LF/HF was significantly higher, suggesting that the sympathetic and vagal balance of patients in the adverse event group was deranged, mainly because the sympathetic tone of patients in the adverse event group was significantly higher than that of patients in the non-adverse event group. The reasons may be considered as multiple. On the one hand, the enhanced sympathetic nerve activity stimulates the release of a large amount of catecholamines, causing a large amount of calcium ion outflow through the CAMP pathway and the β1 adrenergic receptor pathway, which in turn leads to ventricular arrhythmia. On the other hand, the activity of sympathetic nerves is enhanced, and the depolarisation and repolarisation of the infarcted myocardium in AMI patients are not synchro-nised with the adjacent normal myocardium, resulting in prolongation of the QT-d interval, which in turn significantly increases the risk of malignant arrhythmias. In addition, SDNN, SDANN, and LF/HF all have high accuracy, sensitivity, and specificity in evaluating autonomic nervous function in patients with normal coronary angiography, which further confirms that HRV-related parameters have a good evaluation function on cardiac autonomic nervous function.
CK-MB is a creatine kinase composed of myocardial proteins whose serum levels are significantly elevated when cardio-myocytes are damaged.12 cTnI is an extracellular transcript of troponin whose serum levels are elevated when AMI occurs and can accurately diagnose AMI.13,14 NT-proBNP, a myocardial-derived neurotrophic factor, is likewise clinically valuable in the diagnosis and prognostic assessment of AMI.15,16 Myocardial injury markers, such as CK-MB, cTnI, and NT-proBNP play an important role in the timely diagnosis and determination of AMI. However, the correlation between these indicators and the risk of short-term adverse endpoint events post-AMI is still subject to some debate. Research by Liu et al. posits that CK-MB, cTnI, and NT-proBNP do not hold significant predictive value for the occurrence of adverse endpoint events following AMI.17 Studies have shown a potential correlation between HRV-related parameters and adverse outcomes in adults with AMI, and their reliability and usefulness as risk markers for adverse outcomes in AMI patients.18-20 The results of this study also showed that either HRV-related parameters alone or myocardial injury markers had a positive effect on the risk of adverse endpoint events in AMI patients. The results of this study also showed that both HRV-related parameters and myocardial injury markers alone have good predictive efficacy for the occurrence of adverse endpoints in AMI patients, but the AUC values were greater for the combined diagnosis of the two methods, suggesting that the combined diagnosis of the two diagnostic methods may have better predictive efficacy.
In previous clinical practice, it is usually assumed that AMI patients with combined DM have a poorer prognosis and increased mortality. However, the present study failed to confirm that DM is an independent risk factor for poor short-term prognosis in AMI patients, considering that it may be related to the following reasons. On the one hand, the hyperglycaemic state of patients with DM leads to persistent damage to vascular endothelial cells and blood in a hypercoagulable state. In contrast, after the patients were admitted to the hospital and underwent standardised glucose-lowering therapy, the majority of patients had their blood glucose values effectively controlled, reducing the hypercoagulable state of the vascular blood. On the other hand, patients with DM tend to be older and have comorbidities, such as hyperlipidaemia, whose prognosis for patients with AMI may be due to a combination of causes. Finally, as a single-centric study, patient selectivity bias may also contribute to the failure of DM to be an independent risk factor for poor short-term prognosis in AMI patients.
This study has several limitations. Firstly, the sample size was relatively small, which may have affected the statistical power of the analysis. Secondly, the study was conducted in a single centre, which may limit the generalisability of the results. Thirdly, the study was retrospective in nature, which may have introduced bias in the data collection and analysis. Future studies with larger sample sizes, multi-centre designs, and prospective data collection are needed to validate the findings of this study.
CONCLUSION
It is not uncommon for patients with AMI to experience short term adverse endpoints even after standardised PCI. However, the patients with decreased SDNN and SDANN tests, increased LF/HF, high expression of myocardial injury markers, and possibility of short-term adverse endpoints should be highly guarded.
ETHICAL APPROVAL:
This study was approved and conducted with the consent of the Medical Ethics Committee of the First Affiliated Hospital of Anhui Medical University.
PATIENTS’ CONSENT:
All participating patients provided their written informed consent.
COMPETING INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
CMW, TTS: Supervise operation, case follow-up, statistical analysis, and manuscript writing.
YL: Supervise operation, case follow-up, and statistical analysis.
WXH: Research design, subject guidance, statistical analysis, and manuscript writing.
All authors approved the final version of the manuscript to be published.
REFERENCES
- Gheini A, Pooria A, Pourya A. Evaluating mortality rate and associated parameters in patients with acute coronary syndrome. Cardiovasc Hematol Disord Drug Targets 2020; 20(3):221-6. doi: 10.2174/1871529X206662007091305 33.
- Fan J, Ma J, Xia N, Sun L, Li B, Liu H. Clinical value of combined detection of CK-MB, MYO, cTnI and plasma NT-proBNP in diagnosis of acute myocardial infarction. Clin Lab 2017; 63(3):427-33. doi: 10.7754/Clin.Lab.2016.160533.
- Soeda T, Okura H, Saito Y, Nakao K, Ozaki Y, Kimura K, et al. Clinical characteristics and in-hospital outcomes in patients aged 80 years or over with cardiac troponin-positive acute myocardial infarction-J-MINUET study. J Cardiol 2021; 77(2):139-46. doi: 10.1016/j.jjcc.2020.08.006.
- Aarsetøy R, Aarsetøy H, Hagve TA, Strand H, Staines H, Nilsen DWT. Initial phase NT-proBNP, but not copeptin and high-sensitivity cardiac troponin-T yielded diagnostic and prognostic information in addition to clinical assessment of out-of-hospital cardiac arrest patients with documented ventricular fibrillation. Front Cardiovasc Med 2018; 5:44. doi: 10.3389/fcvm.2018.00044.
- Feng J, Wang A, Gao C, Zhang J, Chen Z, Hou L, et al. Altered heart rate variability depend on the characteristics of coronary lesions in stable angina pectoris. Anatol J Cardiol 2015; 15(6):496-501. doi: 10.5152/akd.2014.5642.
- Damman P, van't Hof AW, Ten Berg JM, Jukema JW, Appelman Y, Liem AH, et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Comments from the Dutch ACS working group. Neth Heart J 2017; 25(3):181-5. doi: 10.1007/s12471-016-0939-y.
- Sethi NJ, Safi S, Korang SK, Hróbjartsson A, Skoog M, Gluud C, et al. Antibiotics for secondary prevention of coronary heart disease. Cochrane Database Syst Rev 2021; 2(2): CD003610. doi: 10.1002/14651858.CD003610.pub4.
- Zhou Y, Liu Y, Zeng R, Qiu W, Zhao Y, Zhou Y. Early long-term low-dosage colchicine and major adverse cardiovascular events in patients with acute myocardial infarction: A systematic review and meta-analysis. Front Cardiovasc Med 2023; 10:1194605. doi: 10.3389/fcvm.2023.1194605.
- Xu H, Faxén J, Szummer K, Trevisan M, Kovesdy CP, Jernberg T, et al. Dyskalemias and adverse events associated with discharge potassium in acute myocardial infarction. Am Heart J 2018; 205:53-62. doi: 10.1016/j.ahj. 2018.06. 009.
- Fitzsimons S, Doughty RN. Role of transthoracic echocardiogram in acute heart failure. Rev Cardiovasc Med 2021; 22(3):741-54. doi: 10.31083/j.rcm2203081.
- Brinza C, Floria M, Covic A, Covic A, Scripcariu DV, Burlacu A. The usefulness of assessing heart rate variability in patients with acute myocardial infarction (HeaRt-V-AMI). Sensors (Basel) 2022; 22(9):3571. doi: 10.3390/s22093571.
- Elcik D, Kelesoglu S, Yilmaz Y, Cetinkaya Z, Sulaiman J, Yurt R, et al. Relationship between thiol, disulphide volume and contrast-induced nephropathy in acute coronary syndrome patients treated with percutaneous coronary intervention. Scand J Clin Lab Invest 2021; 81(3):173-80. doi: 10.1080/ 00365513.2021.1878386.
- Yuan Z, Wang L, Chen J, Su W, Li A, Su G, et al. Electrochemical strategies for the detection of cTnI. Analyst 2021; 146(18):5474-95. doi: 10.1039/d1an00808k.
- Chaulin AM. Some common causes of false positive increases in serum levels of cardiac troponins. Curr Cardiol Rev 2022; 18(6):e130422203527. doi: 10.2174/1573403X 18666220413124038.
- Khan S, Rasool ST. Current use of cardiac biomarkers in various heart conditions. Endocr Metab Immune Disord Drug Targets 2021; 21(6):980-93. doi: 10.2174/1871530320999 200831171748.
- Radosavljevic-Radovanovic M, Radovanovic N, Vasiljevic Z, Marinkovic J, Mitrovic P, Mrdovic I, et al. Usefulness of NT-proBNP in the follow-up of patients after myocardial infarction. J Med Biochem 2016; 35(2):158-65. doi: 10.1515/jomb-2016-0003.
- Liu L, Li S, Ding X, Wang D, Li W, Li H. Dynamic changes in soluble suppression of tumorigenicity 2 levels predict major adverse cardiovascular events in patients with ST‑segment elevation myocardial infarction. Pol Arch Intern Med 2022; 132(10):16317. doi: 10.20452/pamw.16317.
- Brinza C, Floria M, Covic A, Covic A, Scripcariu DV, Burlacu A. The usefulness of assessing heart rate variability in patients with acute myocardial infarction (HeaRt-V-AMI). Sensors (Basel) 2022; 22(9):3571. doi: 10.3390/s220 93571.
- Zhang Y, Wang J, Xu Y. Value of heart rate variability on dynamic electrocardiogram in predicting ventricular fibrillation in elderly acute myocardial infarction patients. Ann Palliat Med 2020; 9(5):3488-94. doi: 10.21037/apm-20- 1362.
- Sagnard A, Guenancia C, Mouhat B, Maza M, Fichot M, Moreau D, et al. Involvement of autonomic nervous system in new-onset atrial fibrillation during acute myocardial infarction. J Clin Med 2020; 9(5):1481. doi: 10.3390/jcm90 51481.